
What happens when the symbiotic relationship between running, diet and maintaining a healthy weight becomes disordered?
By Adrian Monti, Runner’s World UK
One of the many benefits of running is that it helps to control body weight. Anything from a couch-to-5K program to a marathon will burn extra calories, which means many of us use running to stay – or get – in shape. For others, fueling our runs helps us to both value a nutritious diet and enjoy loading up the tank, guilt-free.
For some, however, it isn’t that simple; the balance between what they eat and how much they exercise can become badly skewed. Instead of running for enjoyment and fitness, the overwhelming reason to clock miles becomes to shed more pounds. Or, rather than using their diet to properly fuel their runs, they limit what they eat to shave weight in pursuit of performance. Taken to extremes, this may become a full-blown eating disorder.
You’ll know something about anorexia, bulimia and binge eating, even if you’re not completely familiar with their symptoms and manifestations. All three – along with other, not-so easily-classified eating disorders – are linked with an abnormal preoccupation concerning food. And, sadly, they are disorders that many people are struggling with. The eating-disorder charity Beat estimates that about 1.25 million people in the UK have an eating disorder.
People with an eating disorder are almost four times more likely to become addicted to exercise
Unfortunately, it’s also common for people with these conditions to look for another way of controlling their body shape–excessive exercise, often involving running. In a study published at the start of this year, researchers from Anglia Ruskin University, in Cambridge, concluded that people with an eating disorder are almost four times more likely to become addicted to exercise. The study found that a high percentage of those who exercised obsessively – meaning it was extreme enough to have a negative effect on their health and social life – did so because they were focused on avoiding weight gain.
For some runners who suffer from disordered eating, the focus is not merely on body shape, but also on how losing weight will improve their running performance. And when this gets out of control, it can lock runners into a cycle of declining weight, performance and health.
However, while running can become part of the problem, it is also, often, part of the solution and for many who find their lives in a downward spiral because of disordered eating, running can play a key role in recovery. Here, with the help of four runners who have been courageous enough to share their stories, we examine some of the sensitive issues around eating disorders and running; to help you spot warning signs in yourself or someone close to you; to offer guidance on finding a way through; and to let you know that if you are suffering, you are not alone.
Extreme measures
Keen, fast and dedicated, Rebecca Quinlan discovered her running talent early. After she joined her local club, when she was 13, her ability as a sprinter won her numerous regional honours and she reached the national championships while still in her teens. ‘I trained almost daily from an early age,’ says Rebecca. ‘I was ranked in the UK top 30 and I dreamt of becoming a professional athlete.’

Fast forward six years and Rebecca was in a much darker place. Weighing close to 5st and with a body mass index (BMI) of 11 – below 18.5 is considered underweight–her ambitions were in tatters as she struggled to walk, never mind run. ‘My eating disorder started when I was around 14,’ she recalls. ‘I was convinced that if I lost weight, I would run faster.’
When Rebecca went to university, things rapidly spun out of control. ‘I hugely cut back on what I ate,’ she says. ‘Soon, I was eating only one small meal a day, of vegetables. I was training with elite runners, so my training was incredibly intense, meaning even more weight dropped off. But rather than making me faster, the more weight I lost, the worse my running became. I could feel my athletics dream was slipping away. It got so bad that I couldn’t run at all, so, instead, I totally focused on losing weight. But after eight months at university, my body began to shut down. I was seriously ill.’
Rebecca’s flatmates were so worried they secretly contacted her parents, who were ‘horrified’ when they saw their emaciated daughter. Rebecca immediately went into intensive care, as her kidneys, liver and heart were failing. She spent most of the next three years in hospital eating-disorder units, where she was tube-fed. ‘I’d dropped out of university, lost touch with friends and my life was taken over by anorexia. I couldn’t see a way out of it,’ she says.
Rebecca’s story is far from unusual. Growing numbers across all age ranges – and a quarter of them male – are being diagnosed with eating disorders. According to NHS Digital data released in January, there has been a 37 per cent increase in hospital admissions for these disorders over the past two years.
Beat’s data shows that eight per cent of those with an eating disorder have anorexia – the most dangerous of the illnesses because of its high mortality rate owing to suicide and fatal complications caused by low weight. Bulimia accounts for 19 per cent of all eating disorders and binge eating, 22 per cent.
Sobering as they are, those figures don’t tell the whole story. ‘There’s a much larger group of people who experience disordered eating,’ says Dr Carolyn Plateau, senior lecturer in sports psychology at Loughborough University. ‘Research suggests around 20 per cent of young females fit into this category. While not as severe as clinical eating disorders, it can still significantly compromise quality of life and can quickly escalate into more severe problems.’ Disordered eating can include, for instance, orthorexia, where someone will only eat so-called ‘clean’, healthy foods regardless of calorie content.
It’s a huge problem, then, and one that runners may be more vulnerable to than most. Plateau says several studies in the past 20 years have shown that athletes – notably those associated with so-called ‘lean sports’ such as long-distance running or cycling – are at a higher risk of disordered eating than the general population. Most of these studies were focused on club, county or elite runners, but Plateau says similar trends can be detected among recreational runners.
Rebecca’s eating disorder developed in her teens, but experts stress it’s not just adolescent females who are affected, as is sometimes believed. Problems occur in much older people and, according to research last year from King’s College London, in younger people, too. Its findings showed a doubling of the rate of anorexia in pre-teens (those aged between eight and 12) in a 10 year period, to 3.2 cases per 100,000 children.
Cause and effect
The underlying causes of eating disorder are, of course, complex. ‘It’s important to recognise that eating disorders do not stem from one factor,’ says Plateau. ‘They’re often the result of an interplay between biological, genetic and environmental factors. It’s very unlikely that sport is ever the sole cause. In some cases, something about running may trigger an eating problem that may have developed anyway. Alternatively, some people who are, perhaps, more vulnerable may turn to running because this environment may help to normalise what might be considered disordered. For example, people with eating problems often exercise to cope with negative emotions, have very rigid exercise routines even when injured and feel guilty about missing a session. And if a running environment endorses these behaviours and/or an individual becomes obsessive or compulsive towards training, then it might be an indicator of a potential eating problem.’
Sports and eating disorder specialist dietitian Renee McGregor, who runs the Bath-based EN:SPIRE clinic and has worked with both Olympic athletes and everyday runners, agrees. ‘Most people with an eating disorder are using food as their coping mechanism rather than, say, alcohol,’ she says. ‘They’re using food as a way of defending themselves from the emotions they don’t want to experience or explore.’
McGregor has also seen how the relationship between eating less and chasing performances can become toxic. ‘In my clinic, I often see runners who are cracking the whip with their training and will eat only as a reward,’ she says. ‘They might start by thinking that shedding some weight will make them quicker, but when this leads to an obsession that being even lighter would make them even faster, things can quickly unravel.’
Various studies have highlighted the prevalence of this damaging pursuit of weight loss for performance gains. A study by sports scientists at Leeds University, for example, which looked at 181 elite female distance runners, found 29 had an eating disorder (seven had anorexia). And McGregor says the issue is not the preserve of the elite-running world, but is common among runners at all levels.
In many cases, the root cause has been hidden for many years, only for running to bring these issues to the surface. ‘Often, runners have an eating disorder as a teenager that was never resolved,’ says McGregor. ‘As adults, it instead becomes a way of coping. So while they run, they’re able to eat more freely, but as soon as they’re injured, the wheels come off and they realise they haven’t dealt with it in the past.’
Positive steps
For some, running can appear to be at the centre of their eating issues, but it can also help them find a way out. At 25, Alex Staniforth, from Kendal, in Cumbria, has already packed an incredible amount into his life. He has attempted to climb Mount Everest twice and taken on several other gruelling endurance challenges, with running always central to his training. But Alex has also suffered from depression from a young age and, since 2012, bulimia and binge eating. ‘A long-term shin injury first stopped me running for a long time and the frustration made me focus instead on food as a way of controlling things,’ says Alex.
While researching healthier eating choices, he began obsessing about everything he put into his mouth. ‘I started cutting out all the so-called “bad” foods,’ he says. ‘I thought I would come back a stronger runner. I didn’t realise it was probably the worst thing I could have done, as it dominated everything. I wasn’t fixated on looking thin–it was to be more like the top runners I admired. I began binge eating thousands of calories and it got worse when I realised I could have my cake and eat it, because, after eating all this food, I would make myself sick. I knew this “solution” was totally wrong, but my eating disorder had me trapped in a dangerous cycle that became wired into my brain. At its worst, food became everything, and I would agonise for hours over what to eat.’
Alex, who is 6ft 4in, was down to 10st (65kg) at his lightest. But once he recovered from his injuries, he returned to running and instead of being part of the problem, his running is now part of the solution. ‘When I can run, my eating issues are kept much more in check,’ says Alex. He has also undergone counselling and learnt techniques to manage his eating disorder. He is now more in control, but he believes it will always be lurking in the background. ‘Running has always been my way of coping with all sorts of issues. The only downside is when I can’t run.’
In the RED
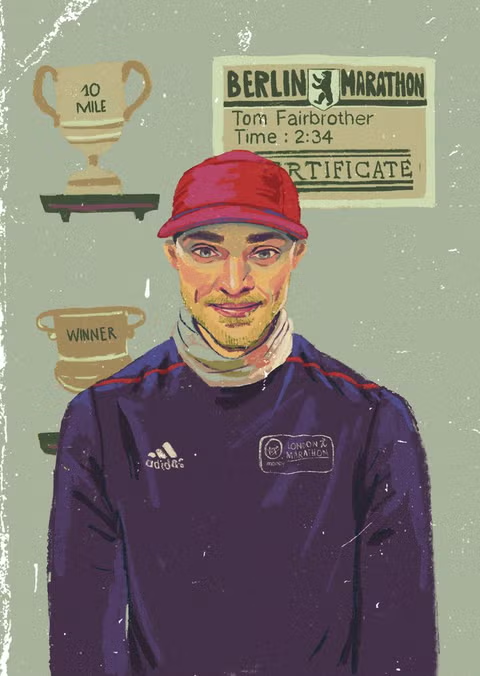
For Tom Fairbrother, his eating disorders were also rooted in his running, but, like Alex, running eventually offered him a way back. After showing potential in his 20s, he decided to step up his running, so he travelled to the high-altitude Kenyan training camp at Iten, where Mo Farah was then based. But his plans were scuppered when he arrived for his three-month stay with a calf injury. ‘It was a culture shock being at the camp where you just ran, ate and slept,’ says Tom. ‘My injury meant I couldn’t run at all and with all these elite runners about, I felt a fraud.’
A coach suggested that if Tom lost a few kilos he would run faster. So, while unable to train, he began skipping meals. Though he returned home after only a month, Tom continued to drastically restrict his food intake and his weight plummeted. When he could finally run again, he lost even more weight. ‘I would run before my breakfast, which I would throw up in the bathroom, go to work, not eat all day, run a second time and again throw up my evening meal,’ says Tom. ‘As I got thinner, I felt I had to run so much to hide my weight loss. I had a mental health illness with a really destructive behaviour I couldn’t stop. I was trapped in a cycle of overexercising and not eating enough. I had anorexia and then bulimia and today I would be seen as textbook example of RED-S.’
Relative Energy Deficiency in Sports, or RED-S, is a new term used to describe a long-standing condition. It develops when someone has insufficient energy to cover the ongoing process of keeping their body’s metabolism functioning, while also adding exercise into the mix. When you don’t consume enough food to fuel both of these demands, the body goes into an energy-saving mode – like an electronic device with a low battery–and begins switching off some of its essential metabolic functions.
In women, this could mean disrupted periods (because the production of the oestrogen hormone is affected) and bones weakening (owing to the reduction in new bone-forming when existing bone suffers microfractures during running). The digestive system can be affected, too. The condition was known as ‘the female athlete triad’ because it was more identifiable in women, but now men are increasingly being diagnosed.
Signs that someone is suffering from RED-S include an increase in injuries, fatigue, recurrent illness and mood changes. In the long term, it can have serious consequences on the cardiovascular system, immunity and, in women, fertility. ‘Insufficient fuelling can make it harder for your body to repair and recover between training sessions, thus increasing the risk of illness and injury,’ says Plateau. ‘RED-S has been widely demonstrated to negatively impact a wide range of body systems, thereby compromising health and performance.’
The bad news is RED-S is becoming an issue in runners of all abilities. As an early warning flag, look for performance stagnating or declining even though training volume is increasing. ‘In females, the menstrual cycle is a good marker to indicate whether you’re getting sufficient energy,’ adds Plateau. ‘If your cycle has recently lengthened or stopped altogether, this may be a sign you’re experiencing RED-S and you should contact your GP. For both sexes, think about whether you’re experiencing constant niggles or illnesses, or have noticed changes in your coordination, concentration or wellbeing. Make a conscious effort to increase your energy intake if you’re upping your mileage or intensity, to make sure your body benefits from your training.’
Tom’s symptoms included poor sleep, hormone disruption, lack of energy and low mood. And despite being lighter, his increased mileage didn’t help his running. For a while, he was able to hide the problem. ‘As runners are seen as skinny, no one questioned why I was so stick-thin because of all my training,’ he says. But, in December 2014, after a routine dental check-up, his dentist asked him if he had an eating disorder. He saw how damaged Tom’s teeth were from stomach acid eroding the enamel after vomiting. This confrontation was a turning point.
As Tom began eating more – only small amounts, at first–he was rewarded with improved running performance, which helped to kick-start a positive cycle. ‘I won a 10-mile race and had much more energy,’ says Tom. ‘It reinforced to me that I needed to eat if I wanted to run better.’ As his weight crept up, his running became more consistent and his performances improved greatly. He set PBs in various distances, including 2:34 at the Berlin Marathon.
He’s now chasing a 2:30 marathon finish. Tom’s guilt about his secret eating disorder eased when he told his parents and friends, who were all supportive. He also benefited from NHS counselling sessions. ‘I still struggle to justify eating some foods if I don’t feel I’ve earned them with a run, so rest days are hard,’ says Tom, now 32, who hasn’t relapsed in almost six years. ‘My wife makes sure I don’t restrict foods and eat more normally. It still makes me angry that our sport believes being lighter makes runners faster – it’s false. That wasn’t the case with me and we need to change that message.’
Taking control
Away from the drive for better performance, running can be a positive force in coping with disordered eating and the underlying psychological issues that may cause it. ‘Running can keep some people going through life by giving them a healthier target rather than an obsessional goal of losing weight,’ says Dr Christian Buckland, a professional adviser to the UK charity Anorexia & Bulimia Care. But he adds the warning that our physical health can be damaged if we exercise at a high intensity while also coping with an eating disorder.
‘It can be a really helpful coping strategy if done safely, but it’s important to weigh up the risks,’ says Buckland. ‘Running can be helpful, but also potentially dangerous for those suffering with an eating disorder, depending on the nature and severity. For example, someone struggling with anorexia or bulimia may find they have developed a heart condition or are prone to weakened bones, which running can exacerbate. So it’s important that if someone has an unhealthy relationship with food, weight or body image, they should consult an eating- disorder specialist to ensure running is safe for them.’
For mother of three Andrea Sexton, from Dursley, in Gloucestershire, running was a major source of help in coping with the anorexia that she developed at 17. ‘It was probably a reaction to being partially deaf, which meant I struggled with friendships,’ says Andrea, now 44. ‘Feeling under pressure with my schoolwork, food became my way of controlling my life when I was feeling overwhelmed. By restricting what to eat, I felt that I was achieving something. Back then, people didn’t talk about eating disorders so much. I remember seeing my former GP, who recommended I simply eat a couple of Mars bars.’
Andrea lost so much weight that she came close to being hospitalised. Her anorexia meant that she didn’t have enough strength for the two things she loved–running and horse riding. But, ultimately, running was her salvation. ‘When I was 21, I went to university, which gave me more structure,’ she recalls. ‘There, I met my future husband, Andy, who did triathlons; he got me interested in how nutrition fuels the body. And this encouraged me to run again and I completed some races.’
She also discovered cognitive behavioural therapy and yoga. Five years ago, she joined her local running club and now enjoys the trails around her Cotswolds home. ‘I’ll always fixate on food but it’s something I’ve learnt to live with. Even now, I follow a strict timetable in my head of when I eat, as my way of dealing with it. But I no longer feel guilt about what I eat compared to when I was younger. Running is my escape, and it’s the wind on my face and the fresh air in my lungs that I love.’
After her final hospital discharge, Rebecca Quinlan began rebuilding her life. She completed her degree and now talks to university students about eating issues. ‘After hitting rock bottom, I realised I wanted more out of life,’ says Rebecca, now 32, who returned to running in 2016. ‘Running was a major player in my eating disorder, as I was feeling a bit left out at school. I was also apprehensive about running again, as it could really help or send me down the same path as before. But training in a group at my old club has helped me recover. I’m now more flexible and run because I want to, not because I have to.’
Like many people who have experienced eating disorders, Rebecca now feels more in control of the forces behind it and that progress is, she says, at least partly due to reconnecting with running. ‘My eating disorder will always be there because it has been in my life for so long, but I’m aware of the triggers and how to manage it.’
For anyone who is struggling with an eating issue, Rebecca’s story shows that, however dark and scary things may seem at times, recovery is possible.